Revolutionizing Endometrial Cancer Diagnosis: What the New Model Brings
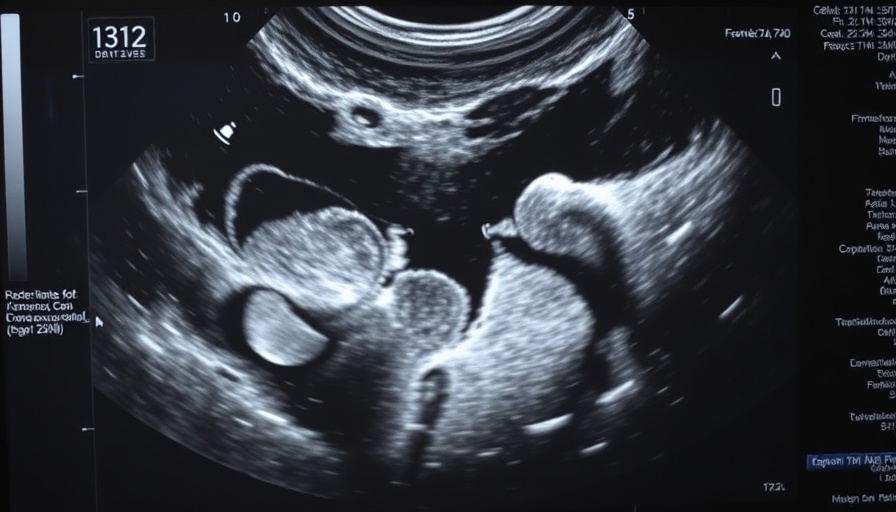
In a promising development for women's health, researchers have unveiled a groundbreaking ultrasound-driven model designed to enhance diagnostic accuracy for endometrial malignancies. This advancement is particularly significant as endometrial cancer is among the most common gynecological cancers globally, yet it often remains misdiagnosed until it has reached later stages. The new approach harnesses advanced imaging technology to improve early detection rates, which can significantly impact treatment outcomes.
The Science Behind the Model: How It Works
The newly developed model employs artificial intelligence algorithms that analyze ultrasound images more effectively than traditional methods. These algorithms are trained on vast datasets, allowing them to recognize subtle patterns and anomalies in tissue that may indicate cancerous changes. This AI-driven process not only increases diagnostic accuracy but also reduces the need for invasive biopsies, providing a non-invasive alternative for patients.
The Impact of Early Detection on Patient Outcomes
Statistics reveal that early-stage diagnosis of endometrial cancer can lead to a survival rate of over 95%. This starkly contrasts with the survival rates for advanced-stage diagnoses, which can plummet to around 15%. By increasing the speed and accuracy of diagnoses, this new model could save lives and alleviate the emotional burden faced by patients and their families. The implications of this technology extend beyond individual health, potentially reducing healthcare costs associated with late-stage cancer treatments.
Broader Implications for Women's Health Technology
This model represents a significant advancement in the integration of technology within women's health care. As AI and machine learning continue to evolve, we can expect to see a burgeoning array of diagnostic tools that empower both clinicians and patients. The health sector is moving toward a more precision-based approach, facilitating better-tailored treatments and more informed patient choices.
Challenges and Counterarguments: A Balanced Perspective
While the advancements are promising, it is essential to consider the existing challenges. Critics argue that reliance on technology can lead to false assurances if not balanced with clinical expertise. Moreover, access to advanced diagnostic technology can vary significantly across different regions, raising questions about health equity. Thus, while the technology represents a leap forward, it must be complemented with strategies to ensure equitable access in diverse healthcare settings.
Future Predictions: What's Next for Ultrasound Technology?
Looking ahead, the potential applications of ultrasound technology in diagnostics are extensive. We anticipate further refinements in AI algorithms that can aid in not just cancer detection but also in the management of other gynecological conditions. Continued interdisciplinary collaboration between software engineers, medical professionals, and researchers will be crucial in driving this field forward.
Empowering Women Through Knowledge
Understanding the advancements in diagnostic technology is invaluable for women, their families, and healthcare providers. Awareness and education about such innovations empower patients to advocate for themselves during medical consultations. Knowledge of available technologies can stimulate dialogue around personalized patient care and informed consent.
Conclusion: The Time for Change is Now
This new ultrasound-driven model is not just a technical improvement; it's a beacon of hope for countless women. As we embrace such technological advancements, the healthcare community must strive to align these innovations with ethical practices that prioritize patient care and equitable access. By investing in these technologies today, we can pave the way for healthier tomorrows.
 Add Row
Add Row  Add
Add 



Write A Comment