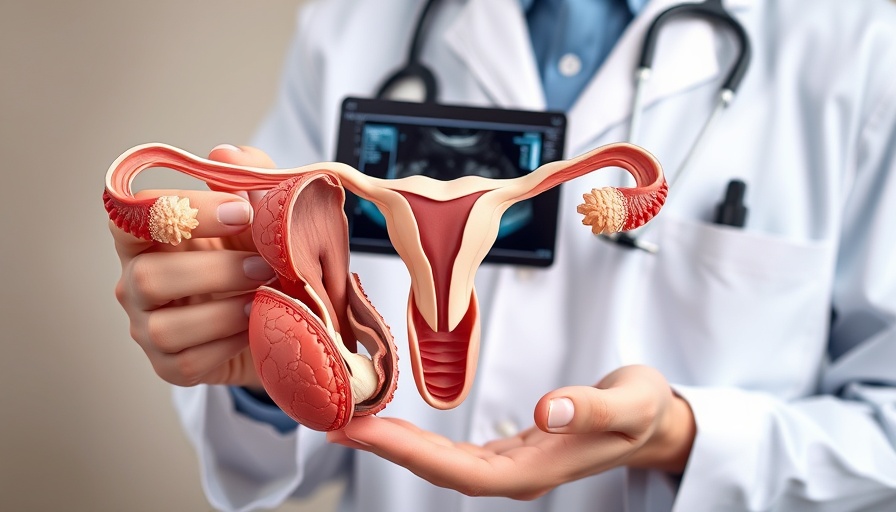
Understanding Cervical Cancer Screening Guidelines
Cervical cancer is a significant health concern that affects women worldwide. According to the American Cancer Society, regular screening can prevent most cervical cancers, yet many women are unsure of when to stop these essential check-ups. A recent study has come under scrutiny, assessing the risks associated with women exiting cervical cancer screening at age 65. As the landscape of healthcare evolves, understanding these parameters is crucial.
Why Exiting Screening at Age 65 is Controversial
Guidelines traditionally recommend that women continue cervical cancer screening until at least age 65 if they have had a history of high-grade lesions or cancers. The study suggests that for many women, exiting screening at this age may seem justified, especially for those who have had consistent negative screenings. However, experts caution against this, pointing out that the risk of new cases and potential late diagnoses increases significantly among older women.
Historical Context and Background
The protocol for cervical cancer screening has gone through numerous transformations over the decades, with a marked emphasis on preventative strategies through Pap smears and HPV testing. Understanding this historical evolution aids in grasping why current recommendations still advocate for screenings past age 65 for those at risk. The implications of these guidelines are further enhanced by rising incidents of HPV-related diseases, requiring women to remain vigilant through their senior years.
The Societal Impact of Cervical Cancer
Cervical cancer is not merely a personal health issue; it affects families and communities at large. According to the CDC, cervical cancer screenings are vital for early detection and treatment, which can help lower mortality rates. Discussions around the cutoff age for screenings can impact numerous women’s health choices, community health programs, and ultimately the burden on healthcare systems. The need to educate women about their health choices after age 65 cannot be overstated.
Risks and Recommendations Post-65
Data indicates that the risk of cervical cancer increases for women who exit screening at 65. The study reveals that skipping these screenings can potentially lead to missed early-stage cancers, putting women at risk without adequate follow-up care. Medical professionals advocate for maintaining regular check-ups, particularly for women with risk factors such as a family history of cervical cancer or past HPV infections.
Future Insights: Trends to Watch
As we move forward, the conversation must shift toward personalized healthcare strategies. The ongoing discussions around the cessation of screenings in older women highlight a need for tailored advice based on individual risk profiles. Future studies should explore the long-term impacts of stopping screenings too soon, as more data emerge from ongoing monitoring of this demographic.
Making Informed Healthcare Decisions
It is essential for women facing the decision of whether to continue or exit cervical screening after age 65 to weigh both their medical history and the advice of healthcare providers. Engaging in open conversations with physicians is vital, as early detection remains a key factor in effectively managing cervical cancer risk.
As the discourse around cervical cancer prevention evolves, women across the globe must remain informed and proactive about their health choices, particularly as they age. If you or someone you know is approaching the age of 65, ensuring a thorough discussion with your healthcare provider about the benefits of continued screenings may be the difference between early detection and late diagnosis.
 Add Row
Add Row  Add
Add 



Write A Comment